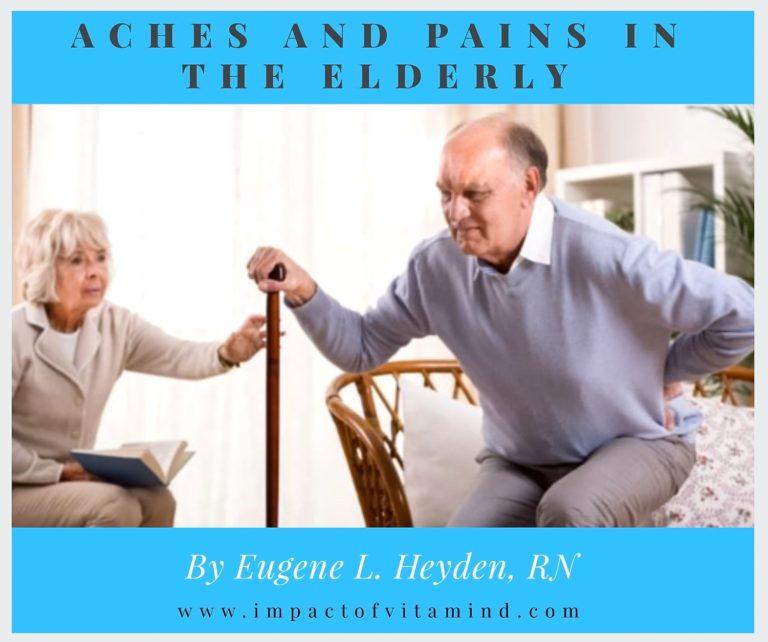
Aches and Pains in the Elderly
Last update: 09-14-22
By Eugene L. Heyden, RN
Aches and pains are so very common, particularly in the elderly. We should do what we can to prevent them. A lot of suffering is associated with aches and pains in this segment of our population. Perhaps surprisingly, vitamin D deficiency could be behind many cases yet to be diagnosed—do you think that guy up there is getting enough vitamin D to keep him out of trouble? (I think not.) In this article we will review three case reports that shed a little sunlight on the issue of vitamin D deficiency and back pain. But back pain isn’t the only thing we will discuss. A variety of aches and pains in the elderly have been linked to vitamin D deficiency. Read and share. I know you have nothing better to do.
Important! As you read the following case reports, keep in mind that a vitamin D level of less than 20–30 ng/ml is probably too low, a vitamin D level below 15–20 ng/ml is way too low, and a vitamin D level below 15 ng/ml is bad news, very bad news. Someone could get hurt.
Back pain
Case #1: Back pain, age 78, long-term, initial vitamin D level of 2.2 ng/ml. Complete resolution occurred within 4 weeks after vitamin D status normalized to 52 ng/ml. (Ghose, 2004a)
Case #2: Back pain, age 86, of three months duration and associated with a history of lumbar compression fractures. Vitamin D level was increased from <5 ng/ml to 36 ng/ml with pain resolution occurring following 3 weeks of treatment. (Ghose, 2004b)
Case #3: Back pain, age 63 (not exactly elderly, but close), with a history of 4 back operations. He received the diagnosis “failed back surgery” and his self-esteem plummeted (well, it probably did). He was on long-term disability and attended a pain management clinic. He was a total mess! “His symptoms completely resolved after six weeks on 4,000 IU of vitamin D [per day] after years of having pain.” His initial vitamin D level was 8 ng/ml. After treatment, his level rose to 34.8 ng/ml. (Schwalfenberg, 2009)
Aches and pains
Who would have guessed, it was vitamin D deficiency behind all the misery outlined above? But if it’s not back pain, you know it will be something else. Next, we’ll focus on other aches and pains commonly found in the elderly.
Case #4: Age 71, history of severe leg pain, muscle weakness, and difficulty walking. Included in his diagnosis was diabetic neuropathy. After treatment that brought his vitamin D level from 11.2 ng/ml to 74.8 ng/ml, “his weakness and bone pains resolved within 6 weeks. He currently walks 2 to 3 blocks on his own without support.” (Prabhala et al., 2000)
Case #5: Age 77, confined to a wheelchair, with a vitamin D level of 4.8 ng/ml. “She was given oral ergocalciferol [D2] (50,000 IU/wk), with a dramatic improvement in her aches and pains. There was improved mobility, decreased weakness, and ability to forsake the wheelchair in 6 weeks.” (Prabhala et al., 2000)
Case #6: Age 67 (pre-elderly), with “severe, painful proximal myopathy at the hip girdle.” This unfortunate lady has a life complicated by metastatic cancer. After being treated with 50,000 IU/wk of D2, her vitamin D level went from 4.8 ng/ml to 16.8 ng/ml. “Her pain and weakness improved significantly in 8 weeks.” (Prabhala et al., 2000)
Now, if that’s not enough suffering to endure in one day, continue reading.
Case #7: Age 86, weak and malnourished. She was admitted to a nursing home with severe lower extremity pain. Her vitamin D level was 5 ng/ml. Twenty some days later, following restorative nutrition along with vitamin D replacement of 700 IU/day, her “pain had subsided completely.” Following treatment, her vitamin D level rose to 35 ng/ml. (Gloth et al., 1991)
Case #8: Age 85 and counting. She was admitted to the nursing home following a 3 month stay in the hospital to undergo treatment for a lung infection. She suffered “intense” pain in both legs and feet. Each leg was tender to the touch. She did not like her feet anymore, for they were not happy feet. Her vitamin D level was 4.1 ng/ml. Following a 50,000 IU dose of oral vitamin D, she reported noticeable improvement in her level of pain. (Gloth et al., 1991)
Case #9: Age 68 (elderly enough). This gentleman was confined at home a number of years to a “dark and dingy bedroom” and was too weak to walk. He would cry out in pain from time to time and avoided all physical activity. Pain limited his mobility and even occurred with a light touch to the skin. His vitamin D level was found to be at 12.8 ng/ml. After one week following an initial
50,000 IU of vitamin D and 400 IU/day, “his pain vanished.” (Gloth et al., 1991)
Case #10: Age 94. This lady had recently suffered a broken hip and was admitted to a nursing home for continuing care. One complaint was severe lower leg pain. Her vitamin D level was a mere 3.2 ng/ml (extremely low). She received both vitamin D and calcium supplementation and, within 5 days, reported improvement, even with only a minor increase of her vitamin D level to 4.4 ng/ml. Her need of pain medication was greatly reduced. (Gloth et al., 1991)
I think 10 case reports is enough—you get the point! Vitamin D deficiency, prolonged and unidentified, could be a common cause of chronic aches and pains in the elderly, back pain included. It certainly looks so. Let’s end with the following two quotations:
“Older adults are at particular risk for vitamin D deficiency due to reduced sun exposure and decreased dietary intake and absorption. In addition, an increase in body fat leads to a larger distribution volume for the fat-soluble 25(OH) D3, which decreases bioavailability. Multiple studies have suggested a correlation between vitamin D deficiency and pain, particularly back and musculoskeletal pain.” (Kessenich, 2010)
“Vitamin D insufficiency is common; repletion of vitamin D to normal levels in patients who have chronic low back pain or have had failed back surgery may improve quality of life or, in some cases, result in complete resolution of symptoms.” (Schwalfenberg, 2009, emphasis added)
Note: In the above case reports, I took the liberty to converting the nmol/L value used, where needed, to the ng/ml equivalent. Since ng/ml is the value that you will most likely see on a laboratory report, this conversion should help you better relate to the above case reports.
Related articles (Click image to open)
References
Ghose R 2004a Osteomalacia: Recovery of Bone Density. Journal of the New Zealand Medical Association; June 18; 117(1196)
Ghose R 2004b Sub-clinical Osteomalacia. Journal of the New Zealand Medical Association; August 20; 117(1200)
Gloth III FM, Lindsay JM, Zelesnick LB, Greenough III WB 1991 Can Vitamin D Produce an Unusual Pain Syndrome? Arch Intern Med; August; 151:1662–1664
Kessenich CR 2010 Vitamin D Deficiency and Leg Pain in the Elderly. The Nurse Practitioner 35(3):12–13
Prabhala A, Garg R, Dandona P 2000 Severe Myopathy Associated with D Deficiency in Western New York. Arch Intern Med; April 24; 160:1199–1203
Schwalfenberg G 2009 Improvement of Chronic Back Pain of Failed Back Surgery with Vitamin D Repletion: A Case Series. J Am Board Fam Med 22:69– 74
Disclaimer: This article is presented solely for informational purposes. The information contained herein should be evaluated for accuracy and validity in the context of opposing data, new information, and the views and recommendations of a qualified health care professional, and not to be substituted for professional judgment and guidance or to provide reason to neglect or delay appropriate medical care. It is the reader and reader only who bears the responsibility for any actions that could be construed as being a response to the information contained herein. The statements and opinions expressed by the author have not been reviewed or approved by the FDA or by any other authoritative body, nor is the author endorsing any product or specific therapy. This article is offered to the reader to broaden his or her understanding of the issues discussed and to help identify options that may be suitable for the individual to pursue, on behalf of self or others, under approval and direction of a qualified physician. The author and publisher offer no guarantees of the accuracy or validity of the quotations incorporated into this article or the accuracy or validity of the information presented by the resources that are herein recommended.
Copyright © 2016–2022 Eugene L. Heyden, RN
All Rights Reserved.